Aneurysm: Understanding the Silent Threat – Causes, Symptoms, Diagnosis, and Treatment
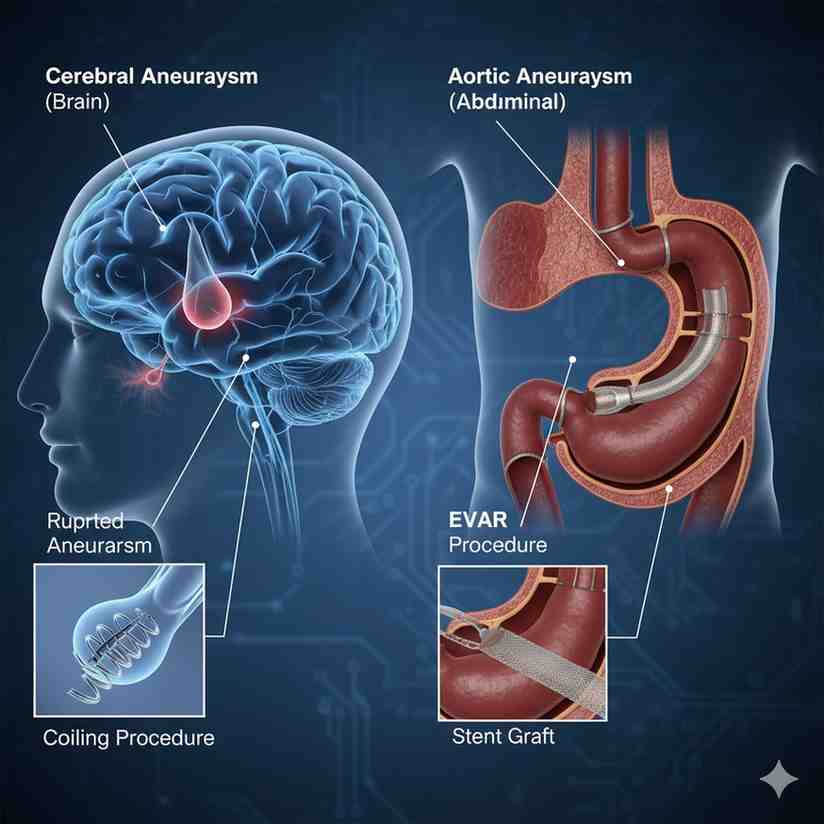
An aneurysm is a bulge or ballooning in the wall of a blood vessel. It’s often described as a weak spot that stretches under the pressure of blood flow. While aneurysms can occur in any blood vessel, they are most dangerous when they affect major arteries, particularly in the brain (cerebral aneurysm) or the body’s main artery, the aorta (aortic aneurysm). When an aneurysm ruptures, it can lead to severe bleeding, stroke, organ damage, or even death, making understanding this condition crucial for everyone.
The danger of an aneurysm lies in its often “silent” nature; many go undetected until they rupture. However, being aware of the risk factors, potential symptoms, and the importance of early diagnosis can make a life-saving difference.
What Causes an Aneurysm?
Aneurysms develop when the pressure of blood flowing through a weakened artery wall causes a section to bulge outwards. Several factors can contribute to this weakening:
- Atherosclerosis: This is the most common cause, where plaque (fatty deposits) builds up in the arteries, making them stiff and weak. High blood pressure then puts additional strain on these weakened areas.
- High Blood Pressure (Hypertension): Chronic high blood pressure significantly increases the force on artery walls, accelerating their weakening and enlargement.
- High Cholesterol: Contributes to atherosclerosis.
- Smoking: Damages blood vessel walls, increases blood pressure, and accelerates atherosclerosis. It’s a major risk factor for all types of aneurysms.
- Family History: A genetic predisposition can increase the risk, especially for brain aneurysms.
- Genetic Conditions: Certain inherited conditions, like Marfan syndrome, Ehlers-Danlos syndrome, and Polycystic Kidney Disease, weaken connective tissues in blood vessels.
- Trauma or Injury: Direct damage to a blood vessel can sometimes lead to an aneurysm.
- Infection (Mycotic Aneurysm): An infection can weaken the artery wall.
- Drug Use: Particularly cocaine and amphetamines, which can drastically raise blood pressure.
Types of Aneurysms and Their Symptoms
The symptoms of an aneurysm depend heavily on its location and whether it has ruptured. Many unruptured aneurysms cause no symptoms at all.
1. Brain Aneurysm (Cerebral Aneurysm)
Often found at the base of the brain.
- Unruptured Symptoms (Rare, but possible if large):
- Pain above or behind one eye.
- Dilated pupil.
- Vision changes (e.g., double vision).
- Numbness or weakness on one side of the face.
- Drooping eyelid.
- Ruptured Brain Aneurysm (Medical Emergency!):
- Sudden, extremely severe headache (“thunderclap headache”) – often described as the “worst headache of my life.”
- Nausea and vomiting.
- Stiff neck.
- Blurred or double vision.
- Sensitivity to light.
- Seizure.
- Loss of consciousness.
2. Aortic Aneurysm
Affects the aorta, the largest artery in the body.
- Abdominal Aortic Aneurysm (AAA): Occurs in the part of the aorta that runs through the abdomen.
- Unruptured Symptoms (Often asymptomatic):
- Deep, constant pain in your abdomen or side of your abdomen.
- A pulsating sensation near your navel.
- Back pain.
- Ruptured AAA (Life-threatening Emergency!):
- Sudden, intense, and persistent abdominal or back pain.
- Sweating.
- Clammy skin.
- Dizziness.
- Nausea and vomiting.
- Rapid heart rate.
- Shock.
- Unruptured Symptoms (Often asymptomatic):
- Thoracic Aortic Aneurysm (TAA): Occurs in the chest.
- Unruptured Symptoms (Often asymptomatic):
- Back pain.
- Cough.
- Hoarseness.
- Shortness of breath.
- Difficulty swallowing.
- Ruptured TAA (Life-threatening Emergency!):
- Sudden, sharp, tearing pain in your chest or upper back.
- Difficulty breathing.
- Difficulty swallowing.
- Shock.
- Unruptured Symptoms (Often asymptomatic):
3. Other Aneurysms
Less common but can occur in the legs (femoral or popliteal aneurysm), spleen (splenic artery aneurysm), or other areas. Symptoms vary by location and often involve pain or a pulsating mass.
Diagnosis: Finding the Silent Threat
Since many aneurysms are asymptomatic until they rupture, diagnosis often occurs incidentally during tests for other conditions or through screening for high-risk individuals.
- Imaging Tests: These are key:
- CT Scan (Computed Tomography): Detailed cross-sectional images.
- MRI (Magnetic Resonance Imaging): Provides detailed images of soft tissues.
- Angiography (CT Angiography, MR Angiography, or Conventional Angiography): Uses contrast dye to visualize blood vessels.
- Ultrasound: Often used for screening abdominal aortic aneurysms, especially in older male smokers.
- Physical Exam: A doctor might detect a pulsating mass in the abdomen for AAA.
Treatment: Managing and Repairing Aneurysms
Treatment options depend on the size, location, symptoms, and risk of rupture.
1. Monitoring (Watchful Waiting)
For small, asymptomatic aneurysms with a low risk of rupture, doctors may recommend regular imaging scans to monitor their size. Lifestyle modifications (quitting smoking, blood pressure control) are crucial.
2. Medical Management
- Blood Pressure Control: Medications to lower and manage high blood pressure are vital.
- Cholesterol Management: Statins to lower cholesterol levels.
- Smoking Cessation: Essential for all patients with an aneurysm.
3. Surgical or Endovascular Repair
For larger aneurysms or those with a higher risk of rupture, intervention is typically recommended.
- Open Surgery:
- Clipping (for brain aneurysms): A neurosurgeon opens the skull, locates the aneurysm, and places a tiny metal clip at its base to stop blood flow into it.
- Open Repair (for aortic aneurysms): A surgeon makes an incision, clamps the aorta, removes the weakened section, and replaces it with a synthetic graft.
- Endovascular Repair: Less invasive procedures, often performed via a catheter inserted into an artery (usually in the groin).
- Coiling (for brain aneurysms): Tiny platinum coils are inserted into the aneurysm to fill it, causing blood to clot and preventing rupture.
- Endovascular Aneurysm Repair (EVAR/TEVAR for aortic aneurysms): A stent graft (a fabric tube supported by a metal mesh) is deployed inside the aorta to reinforce the weakened section and redirect blood flow through the graft, bypassing the aneurysm.
Conclusion: Early Detection is Key
An aneurysm is a serious medical condition, but understanding its nature is the first step towards managing the risk. While many remain silent, the sudden onset of a severe headache or excruciating chest/abdominal pain should always prompt immediate emergency medical attention, as these can be signs of a ruptured aneurysm. Regular check-ups, managing risk factors, and adhering to medical advice are crucial for individuals with known aneurysms or those at high risk.